- Your cart is empty
- Continue Shopping
Quick Answer: BLS Definition
Basic Life Support (BLS) is a set of essential emergency medical procedures designed to maintain circulation, breathing, and brain function in individuals experiencing cardiac arrest or other life-threatening emergencies. BLS includes chest compressions, rescue breathing, airway management, and automated external defibrillator (AED) use until advanced medical care arrives.
Key BLS components: Scene safety assessment, CPR (cardiopulmonary resuscitation), AED operation, airway management, and emergency medical services (EMS) activation.
What Does BLS Stand For in Medical Terms?
BLS stands for Basic Life Support – the fundamental emergency care techniques used to sustain life during critical medical emergencies. In healthcare settings, BLS represents the first level of medical care provided before advanced cardiac life support (ACLS) or other specialized interventions.
BLS meaning in medical context:
- Basic: Fundamental, essential techniques anyone can learn
- Life: Focused on preserving vital organ function
- Support: Temporary assistance until professional medical care
Not to be confused with: Bureau of Labor Statistics (BLS.gov) – the federal statistical agency
BLS vs CPR: Understanding the Difference
What is BLS vs CPR?
BLS is comprehensive emergency care that includes CPR as one component, while CPR focuses specifically on chest compressions and rescue breathing.
BLS includes:
- Scene safety assessment
- CPR (chest compressions + rescue breathing)
- AED use and operation
- Airway management techniques
- Emergency response coordination
- Multiple victim management
CPR includes:
- Chest compressions (100-120 per minute)
- Rescue breathing (mouth-to-mouth)
- Hand placement and technique
- Compression-to-breath ratios
Professional distinction: Healthcare providers typically require BLS certification, while general public often learns CPR basics.
The 5 Essential BLS Steps: Complete Assessment Protocol
Step 1: Scene Safety Assessment
Before approaching any victim, always assess scene safety first.
Safety checklist:
- Environmental hazards: Fire, smoke, electrical wires, traffic
- Personal safety: Gloves, protective equipment if available
- Victim assessment: Multiple victims, mechanism of injury
- Bystander management: Clear space for emergency response
Critical point: Never compromise your safety – injured rescuers cannot help victims.
Step 2: Check Responsiveness and Breathing
Determine if the victim requires immediate intervention.
Assessment technique:
- Tap shoulders firmly and shout “Are you okay?”
- Look for chest rise for no more than 10 seconds
- Check for pulse at carotid artery (healthcare providers)
- Assess consciousness level – alert, verbal, painful, unresponsive
Decision point: If unresponsive and not breathing normally, begin CPR immediately.
Step 3: Activate Emergency Medical Services (EMS)
Call for professional help and additional resources.
EMS activation priorities:
- Call 911 immediately (or local emergency number)
- Request AED if not immediately available
- Provide location and nature of emergency
- Stay on line for dispatcher instructions
Team approach: Assign specific person to call EMS while others begin CPR.
Step 4: Perform High-Quality CPR
Maintain circulation and oxygenation through chest compressions and rescue breathing.
Adult CPR technique:
- Hand placement: Lower half of breastbone, between nipples
- Compression depth: At least 2 inches, no more than 2.4 inches
- Compression rate: 100-120 per minute
- Complete recoil: Allow full chest expansion between compressions
- Minimized interruptions: Less than 10 seconds between cycles
Compression-to-breath ratio:
- Untrained rescuers: Hands-only CPR (compressions only)
- Trained rescuers: 30 compressions to 2 rescue breaths
- Healthcare providers: May use bag-mask ventilation
Step 5: Deploy AED When Available
Use automated external defibrillator to analyze heart rhythm and deliver shock if needed.
AED deployment steps:
- Power on AED and follow voice prompts
- Expose chest – remove clothing, dry if wet
- Apply pads according to diagram instructions
- Ensure clear area – no one touching victim
- Follow prompts for analysis and shock delivery
- Resume CPR immediately after shock
AED integration: Continue 2-minute CPR cycles between AED analyses until EMS arrives.
When to Use BLS: Emergency Situations Requiring Immediate Action
Primary BLS Indications
1. Cardiac Arrest
- Signs: Unresponsive, no normal breathing, no pulse
- Action: Immediate CPR and AED deployment
- Outcome: Early CPR can double or triple survival rates
2. Respiratory Arrest
- Signs: Breathing stopped but pulse present
- Action: Rescue breathing, airway management
- Monitoring: Check pulse every 2 minutes
3. Choking (Severe Airway Obstruction)
- Conscious victim: Heimlich maneuver (abdominal thrusts)
- Unconscious victim: CPR with airway checks
- Infants: Back blows and chest thrusts
Secondary BLS Scenarios
4. Near-Drowning
- Remove from water safely
- Begin CPR if no pulse/breathing
- Suspect cervical spine injury
5. Drug Overdose
- Scene safety (unknown substances)
- CPR for respiratory depression
- Consider naloxone if opioid suspected
6. Severe Allergic Reactions (Anaphylaxis)
- Administer epinephrine if available
- CPR for cardiac arrest
- Airway management for swelling
7. Electrical Shock
- Ensure power source disconnected
- Check for burns, cardiac arrest
- Standard BLS protocols apply
8. Severe Trauma
- Control bleeding while maintaining CPR
- Suspect spinal injuries
- Focus on airway and circulation
BLS Procedures: Step-by-Step Implementation
Adult BLS Sequence
Assessment Phase (First 10 seconds)
- Scene safety check
- Tap and shout for responsiveness
- Look for breathing (chest rise)
- Check carotid pulse (healthcare providers only)
Action Phase
- If responsive but distressed: Provide comfort, monitor closely
- If unresponsive with pulse: Rescue breathing at 10-12 breaths/minute
- If unresponsive without pulse: Begin CPR immediately
CPR Technique
- Position: Victim on back on firm surface
- Hand placement: Heel of one hand on lower breastbone, second hand interlaced
- Body position: Arms straight, shoulders over hands
- Compression: Push hard, push fast, full recoil
- Count rhythm: “1 and 2 and 3…” up to 30
Rescue Breathing (if trained)
- Open airway: Head tilt, chin lift
- Seal mouth: Cover mouth completely
- Give breath: 1 second duration, watch chest rise
- Two breaths: After every 30 compressions
Pediatric BLS Modifications
Children (1-8 years)
- One or two hands for compressions (based on child size)
- Compression depth: At least 1/3 chest depth (about 2 inches)
- Same rate: 100-120 compressions per minute
- 30:2 ratio: For single rescuer
Infants (under 1 year)
- Two-finger technique: Middle and ring finger on lower breastbone
- Compression depth: At least 1/3 chest depth (about 1.5 inches)
- Different ratio: 30:2 for single rescuer, 15:2 for two rescuers
BLS Training and Certification Requirements
Professional BLS Certification
Healthcare Provider BLS:
- Duration: Typically 2-4 hours initial training
- Content: Adult, child, infant CPR, AED use, team dynamics
- Certification period: 2 years
- Recertification: Required before expiration
Target audience:
- Doctors, nurses, paramedics
- Dental professionals, pharmacists
- Healthcare students
- Emergency medical technicians
Public Access BLS Training
Community CPR/AED Training:
- Duration: 2-3 hours
- Focus: Basic CPR, AED use, choking relief
- Certification: Often includes wallet card
- Refresher: Annual training recommended
Training providers:
- American Heart Association CPR courses
- American Red Cross programs
- Local fire departments
- Community health organizations
Online vs. Hands-On Training
Blended learning approach:
- Online portion: Theory, videos, knowledge checks
- Skills testing: In-person demonstration required
- Certification validity: Same as traditional classroom training
Pure online limitations: Cannot replace hands-on skills practice for healthcare providers
BLS Equipment and Technology Integration
Essential BLS Equipment
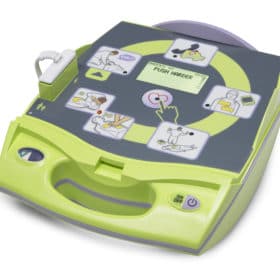
1. Automated External Defibrillators (AEDs)
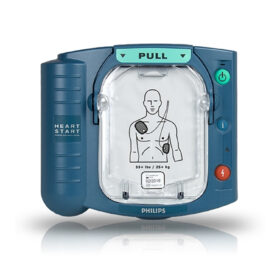
Recommended models:
- Philips HeartStart OnSite AED M5066A: Ideal for workplace and community use
- ZOLL AED Plus: Real-time CPR feedback technology
- Philips HeartStart FRx AED: Rugged design for harsh environments
AED integration with BLS:
- Deploy immediately when available
- Follow device prompts precisely
- Continue CPR between analyses
- Minimize interruptions
2. Barrier Devices and PPE
- Face masks with one-way valves
- Pocket masks for rescue breathing
- Protective gloves (latex-free options)
- Eye protection for body fluid exposure
3. Bag-Mask Ventilation (Healthcare Settings)
- Higher oxygen delivery than mouth-to-mouth
- Two-person technique often preferred
- Requires training for effective use
BLS Technology Advances
CPR Feedback Devices:
- Real-time compression depth monitoring
- Metronome for rate guidance
- Visual indicators for technique improvement
Mobile AED Programs:
- Smartphone apps for AED location
- GPS-enabled emergency response
- Integration with EMS dispatch systems
Legal and Ethical Considerations in BLS
Good Samaritan Laws
Legal protection for BLS providers:
- Coverage: Volunteers acting in good faith
- Scope: Emergency situations, no compensation
- Requirements: Care within training level
- Variations: Laws vary by state/jurisdiction
Key principles:
- Act reasonably and prudently
- Don’t exceed training scope
- Obtain consent when possible
- Continue care until EMS arrives
Consent and BLS
Implied consent:
- Unconscious adults presumed to consent
- Life-threatening emergencies
- Good Samaritan protection applies
Expressed consent:
- Required for conscious adults
- May be verbal or written
- Can be withdrawn at any time
Special populations:
- Minors: Parent/guardian consent preferred
- Mental impairment: Use best judgment
- DNR orders: Honor if valid and present
Professional Duty to Act
Healthcare providers: Legal and ethical obligation to assist within scope of practice
Off-duty considerations:
- Moral obligation vs. legal requirement
- Professional liability concerns
- Good Samaritan protection typically applies
BLS Quality Improvement and Team Dynamics
High-Performance Team BLS
Team roles and responsibilities:
- Team leader: Coordinates care, makes decisions
- Compressor: Provides chest compressions
- Ventilator: Manages airway and breathing
- AED operator: Deploys and operates defibrillator
- Communicator: Liaison with EMS dispatch
Effective communication:
- Clear, direct commands
- Closed-loop communication
- Role rotation to prevent fatigue
- Debriefing after resuscitation
Quality Metrics in BLS
CPR quality indicators:
- Compression rate: 100-120 per minute
- Compression depth: 2-2.4 inches for adults
- Complete recoil: Full chest expansion
- Minimal interruptions: <10 seconds
- Compression fraction: >80% of resuscitation time
Performance monitoring:
- Real-time feedback devices
- Post-event data review
- Continuous quality improvement
- Regular skills assessment
BLS in Different Settings
Community BLS Programs
Public access defibrillation:
- AEDs in schools, offices, gyms
- Trained staff available 24/7
- Clear signage and accessibility
- Regular maintenance and testing
- Employee CPR/AED training
- Emergency response teams
- Coordination with local EMS
- OSHA compliance considerations
Healthcare Facility BLS
Hospital-based BLS:
- Rapid response teams
- Code blue protocols
- Advanced equipment availability
- Transition to ACLS/PALS
Outpatient settings:
- Dental offices, clinics
- Limited advanced equipment
- EMS activation protocols
- Staff training requirements
Transportation BLS
Aircraft medical emergencies:
- Limited space and equipment
- Crew training requirements
- Ground medical consultation
- Emergency landing decisions
Ground transportation:
- Ambulance BLS protocols
- Inter-facility transfers
- Equipment standardization
- Communication with receiving facility
Special Populations and BLS Modifications
Pregnancy and BLS
Maternal cardiac arrest considerations:
- Position: Left lateral tilt if possible
- Compression location: Slightly higher on chest
- Perimortem cesarean: Consider after 4 minutes
- Two-patient approach: Mother and fetus
Geriatric BLS Considerations
Age-related modifications:
- Rib fractures: Common but don’t stop compressions
- Medication effects: May affect response
- Comorbidities: Multiple medical conditions
- DNR status: Verify and honor if present
Pediatric BLS Special Considerations
Anatomical differences:
- Larger head relative to body
- Smaller airway diameter
- Higher respiratory rate
- Different compression techniques
Common pediatric emergencies:
- Respiratory arrests more common than cardiac
- Choking incidents frequent
- Drowning and poisoning
- SIDS considerations for infants
BLS Research and Evidence-Based Updates
Recent BLS Guideline Changes
2020 AHA Guidelines Updates:
- Hands-only CPR emphasis for untrained bystanders
- High-quality compressions priority over ventilation
- AED use encouraged for all age groups
- Team-based approach in healthcare settings
Emerging research areas:
- Mechanical CPR devices
- Extracorporeal CPR (eCPR)
- Targeted temperature management
- Community response optimization
Outcome Studies and Effectiveness
BLS survival statistics:
- Bystander CPR: Doubles or triples survival rates
- AED use: Significantly improves outcomes
- Response time: Critical factor in survival
- Quality training: Improves technique and confidence
Frequently Asked Questions About BLS
Training and Certification
Q: Who should learn BLS? A: Anyone can benefit from BLS training, but it’s especially important for healthcare providers, teachers, coaches, lifeguards, childcare workers, and family members of high-risk individuals.
Q: How often do I need to recertify in BLS? A: Most BLS certifications expire every 2 years. Healthcare providers typically need formal recertification, while community members should refresh skills annually.
Q: Is BLS the same as CPR certification? A: BLS is more comprehensive than basic CPR. BLS includes CPR plus AED use, advanced airway management, and team-based resuscitation techniques.
Legal and Safety
Q: Can I be sued for performing BLS? A: Good Samaritan laws protect individuals who provide emergency care in good faith. However, laws vary by location, so understand your local protections.
Q: What if I’m not certified but need to help? A: Call 911 first, then provide any assistance you can safely give. Many 911 dispatchers can guide you through CPR steps over the phone.
Q: Should I stop BLS if the person has a DNR (Do Not Resuscitate) order? A: If you can verify a valid DNR order, honor it. When in doubt, provide care until EMS arrives and can make the determination.
Technique and Equipment
Q: What if I crack ribs during chest compressions? A: Rib fractures can occur during CPR, especially in elderly patients. Continue compressions – rib fractures heal, but brain death does not.
Q: Can I use an AED on someone with a pacemaker? A: Yes, but avoid placing AED pads directly over the pacemaker device. Place pads at least 1 inch away from the implanted device.
Q: How do I know if my BLS is working? A: Look for chest rise with rescue breaths, check for pulse return every 2 minutes (healthcare providers), and continue until EMS arrives or the person recovers.
Conclusion: The Life-Saving Impact of BLS
Basic Life Support represents the critical bridge between medical emergency onset and professional medical care arrival. Effective BLS can mean the difference between life and death, recovery and permanent disability, hope and tragedy.
Key takeaways:
- Anyone can learn BLS techniques with proper training
- Early intervention dramatically improves survival outcomes
- Quality matters more than perfect technique
- Regular practice maintains skills and confidence
- Equipment accessibility enhances community response
Take action today: Get BLS certified and help create a community prepared to save lives when every second counts.
Philips HeartStart FRx AED with FREE Carry Case 861304
Frequently Asked Questions about BLS
Who should learn BLS? BLS is a critical skill that can be learned by anyone, including healthcare professionals, first responders, lifeguards, teachers, coaches, and anyone else who may find themselves in a situation where they need to provide lifesaving care.
How do I get certified in BLS? Certification in BLS can be obtained through courses offered by organizations such as the American Heart Association (AHA) and the American Red Cross. These courses typically include hands-on training in CPR, AED use, and other basic life support techniques.
Is BLS different from first aid? Yes, BLS is a specialized form of first aid that involves providing immediate care to someone who is experiencing a life-threatening emergency. First aid, on the other hand, is a broader term that refers to any medical care provided to someone before professional medical help arrives.
Can I be held liable if I perform BLS incorrectly? Good Samaritan laws provide legal protection for individuals who provide emergency medical care in good faith, but they may vary from state to state. However, if you are trained in BLS and provide care that is outside of your scope of practice or training, you may be held liable for any harm that results from your actions.
How effective is BLS in saving lives? BLS can be highly effective in saving lives when it is administered quickly and correctly. When performed properly, CPR and AED use can help maintain vital blood flow to the heart, brain, and other organs until professional medical help arrives, which can significantly increase the chances of a successful outcome in a cardiac emergency.